- Article
- Source: Campus Sanofi
- 23 Oct 2023
ESC/EAS DYSLIPIDAEMIA GUIDELINE INTERACTIVE (2 MINUTES)
Treating dyslipidaemia reduces CV risk
Increased LDL-C raises the risk of ASCVD. Lowering LDL-C reduces the risk of future CV events, with no lower limit (no ‘J’ curve effect) and no effect on clinical safety observed to date. ASCVD prevention in the general population starts with promoting healthy lifestyle behaviour; individuals must tackle unhealthy lifestyles and reduce causal CV risk factors, such as LDL-C or blood pressure. The currently available therapies that raise HDL-C do not reduce the risk of ASCVD.
Three steps of treating dyslipidaemia
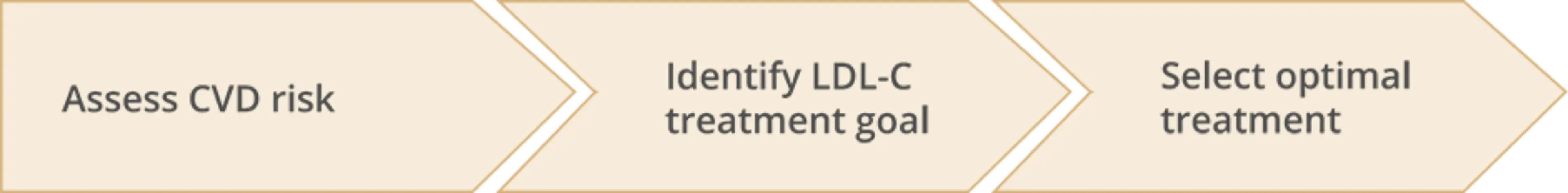
Assess CVD risk
Evaluate clinical risk factors
Total CV risk is very high or high if the patient has any of:
- Documented ASCVD
- T1DM or T2DM
- CKD
These patients do not need a risk estimation model: they all need active management of all risk factors
Formal risk estimation of total CV risk
- For apparently healthy people
- Combining several risk factors can result in high levels of CV risk
- Use a system such as SCORE
Consider additional modifiers that increase risk
- Social deprivation
- Obesity/central obesity
- Major psychiatric disorders
- Psychosocial stress including vital exhaustion
- Non-alcoholic fatty liver disease
- HIV treatment
- Chronic IMID
- Atrial fibrillation
- Obstructive sleep apnoea
- LVH
- CKD
- Physical inactivity
A total CV risk estimate is part of a continuum. Even patients at moderate risk should receive advice regarding lifestyle changes and may require drug therapy.
Identify LDL-C treatment goal
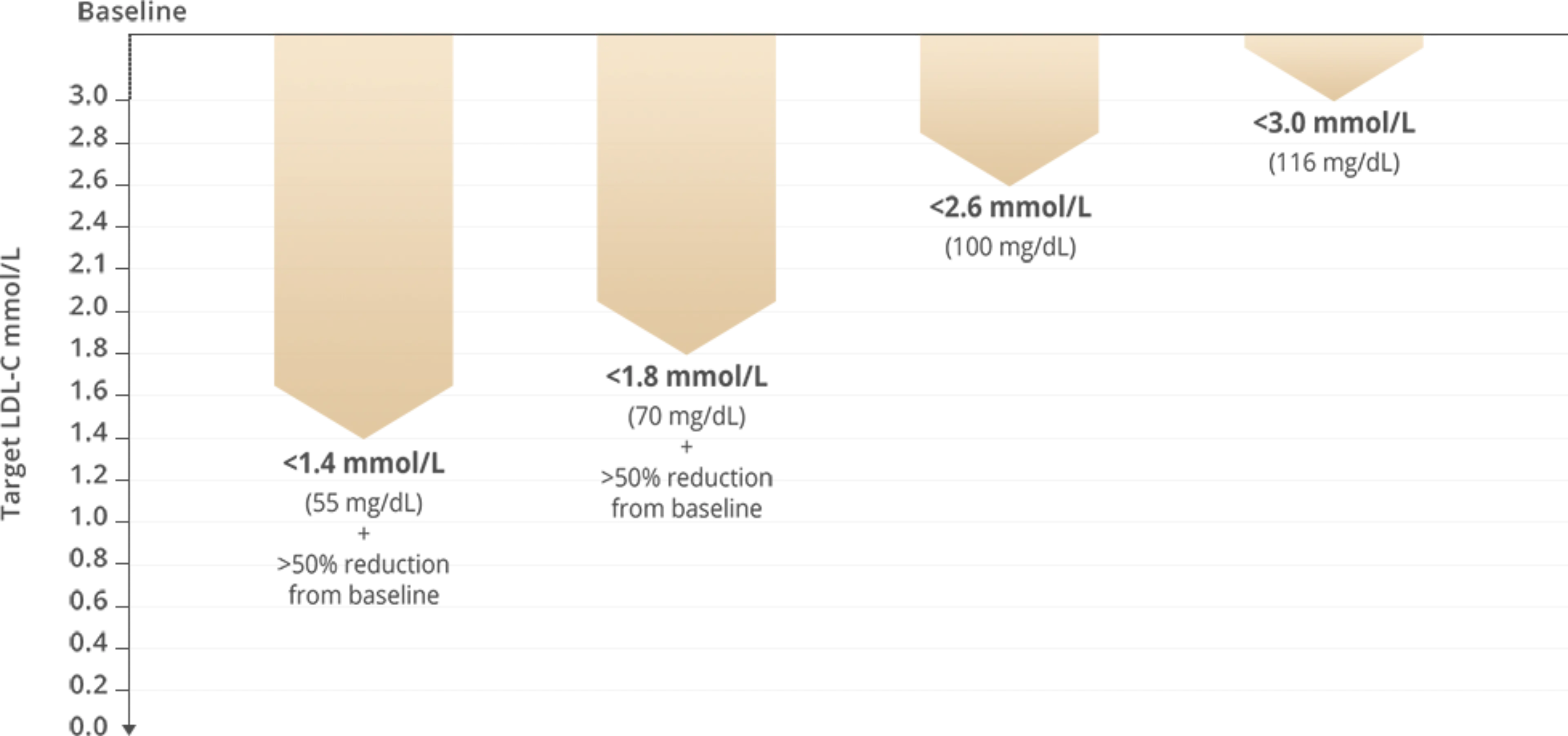
- ASCVD (clinical or imaging)
- SCORE ≥10%
- FH with ASCVD or with another major risk factor
- Severe CKD (eGFR <30 mL/min)
- DM with target organ damage; ≥3 major risk factors; or early onset of T1DM of long duration (>20 years)
- SCORE ≥5% and <10%
- Markedly elevated single risk factors, in particular TC >8 mmol (310 mg/dL) or LDL-C >4.9 mmol/L (190 mg/dL) or BP ≥180/110 mmHg
- FM without other major risk factors
- Moderate CKD (eGFR 30–59 mL/min)
- DM without target organ damage, with DM duration ≥10 years or other additional risk factor
- SCORE ≥1% and <5%
- Young patients (T1DM <35 years; T2DM <50 years) with DM duration <10 years without other risk factors
- SCORE <1%
- ASCVD (clinical or imaging)
- SCORE ≥10%
- FH with ASCVD or with another major risk factor
- Severe CKD (eGFR <30 mL/min)
- DM with target organ damage; ≥3 major risk factors; or early onset of T1DM of long duration (>20 years)
- SCORE ≥5% and <10%
- Markedly elevated single risk factors, in particular TC >8 mmol (310 mg/dL) or LDL-C >4.9 mmol/L (190 mg/dL) or BP ≥180/110 mmHg
- FM without other major risk factors
- Moderate CKD (eGFR 30–59 mL/min)
- DM without target organ damage, with DM duration ≥10 years or other additional risk factor
- SCORE ≥1% and <5%
- Young patients (T1DM <35 years; T2DM <50 years) with DM duration <10 years without other risk factors
- SCORE <1%
Graphic adapted from 2019 ESC Guidelines for the management of dyslipidaemias: lipid modification to reduce cardiovascular risk. European Heart Journal 2019; 41(1): 111-188
Select the optimal treatment strategy for lowering LDL-C
Treatment pathway for pharmacological low-density lipoprotein cholesterol lowering
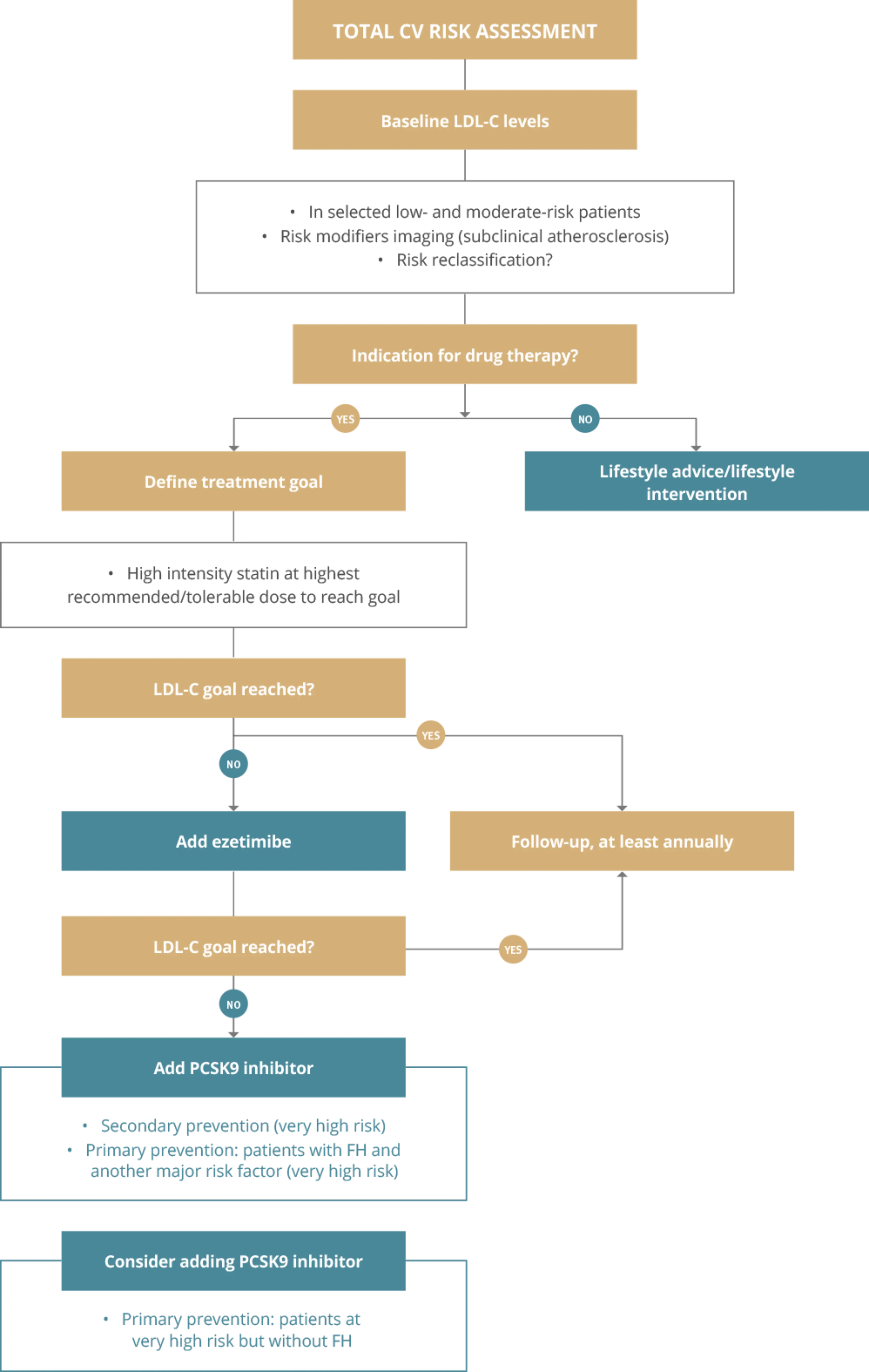
* Please refer to the "risk table" for further information. PSCK9i are licensed for patients with established CVD.
Please refer to individual SmPCs for further information
Graphic adapted from 2019 ESC Guidelines for the management of dyslipidaemias: lipid modification to reduce cardiovascular risk. European Heart Journal 2019; 41(1): 111-188
Section abbreviations
ApoB, apolipoprotein-B; ASCVD, atherosclerotic cardiovascular disease; BP, blood pressure; CKD, chronic kidney disease; CV, cardiovascular; DM, diabetes mellitus; EAS, European Atherosclerosis Society; eGFR, estimated glomerular filtration rate; ESC, European Society of Cardiology; FH, familial hypercholesterolaemia; HIV, human immunodeficiency virus; IMID, immune-mediated inflammatory disorder; LDL-C, low-density lipoprotein cholesterol; LVH, left ventricular hypertrophy; PCSK9, proprotein convertase subtilisin/kexin type 9; SCORE, Systematic Coronary Risk Estimation; SmPC, summary of product characteristics; T1DM, type 1 diabetes mellitus; T2DM, type 2 diabetes mellitus; TC, total cholesterol.

© The European Society of Cardiology and the European Atherosclerosis Association 2019. All rights reserved. For permissions please email: journals.permissions@oup.com.
This publication is for personal and educational use only. No commercial use is authorized. No part of this publication or the original ESC/EAS Guidelines from which it is derived may be translated or reproduced in any form without written permission from the ESC. Permission may be obtained upon submission of a written request to Oxford University Press, the publisher of the European Heart Journal and the party authorized to handle such permissions by the ESC. Sanofi has obtained permission to publish this material and to distribute it to health professionals within France, Spain, IE, Norway, Greece, Croatia, Slovenia, United Kingdom.
Disclaimer:
The ESC/EAS Guidelines represent the views of the ESC/EAS and were produced after careful consideration of the scientific and medical knowledge and the evidence available at the time of their dating. The ESC/EAS is not responsible in the event of any contradiction, discrepancy and/or ambiguity between the ESC/EAS Guidelines and any other official recommendations or guidelines issued by the relevant public health authorities, in particular in relation to good use of health care or therapeutic strategies. Health professionals are encouraged to take the ESC/EAS Guidelines fully into account when exercising their clinical judgment as well as in the determination and the implementation of preventive, diagnostic or therapeutic medical strategies. However, the ESC/EAS Guidelines do not override in any way whatsoever the individual responsibility of health professionals to make appropriate and accurate decisions in consideration of each patient’s health condition and in consultation with that patient and the patient's caregiver where appropriate and/or necessary. Nor do the ESC/EAS Guidelines exempt health professionals from taking careful and full consideration of the relevant official updated recommendations or guidelines issued by the competent public health authorities in order to manage each patient’s case in light of the scientifically accepted data pursuant to their respective ethical and professional obligations. It is also the health professional’s responsibility to verify the applicable rules and regulations relating to drugs and medical devices at the time of prescription.
Reproduced from: Mach F, Baigent C, Catapano AL, et al, 2019 ESC/EAS Guidelines for the management of dyslipidaemias: lipid modification to reduce cardiovascular risk: The Task Force for the management of dyslipidaemias of the European Society of Cardiology (ESC) and European Atherosclerosis Society (EAS), European Heart Journal 2020; 41 (1): 111–188, doi:10.1093/eurheartj/ehz455. With permission of Oxford University Press on behalf the European Society of Cardiology.
Please visit: https://www.escardio.org/Guidelines/Clinical-Practice-Guidelines/Dyslipidaemias-Management-of
Sanofi was not involved in the development of this ESC Guideline and in no way influenced its content.
MAT-XU-2204595 (v3.0) Date of Preparation: October 2023
